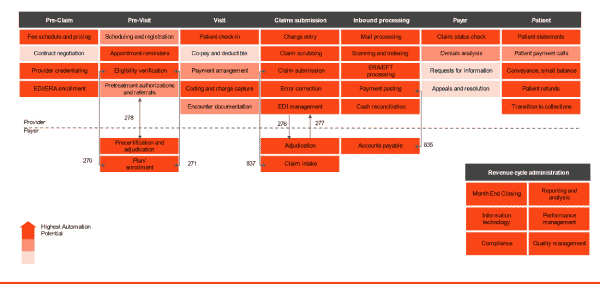
Download Process Heatmap
Mitigate errors, reduce denials, and serve patient data with speed and accuracy – all thanks to KeyMark's RCM automated solutions.
Learn more about your Healthcare Revenue Cycle processes ripe for automation!
You care about patients. But, if you don’t make your revenue goals, it doesn’t matter how much you care.
Fortunately, we care about helping you manage your revenue cycle! We know the tangled web that is the healthcare revenue cycle. And, from pre-registration to collections, we understand the complexities of what your team is facing, and how technology can not only make things easier, but faster, more accurate, and more fair for everyone.
How you maximize revenue capture has changed. You’re probably not doing random chart audits anymore.
Instead, today you’re looking to data analytics for answers. KeyMark is all about automating the things that we can, to free you up for the things that matter. As your partner in healthcare technology, we want to show you a path to leveraging the very latest technologies like Robotic Process Automation (RPA) to streamline your workflows, connect your information silos, and empower your people to drive both patient satisfaction AND cost efficiencies at every step of the revenue lifecycle.
Automation Can Transform These Steps In Your Revenue Lifecycle
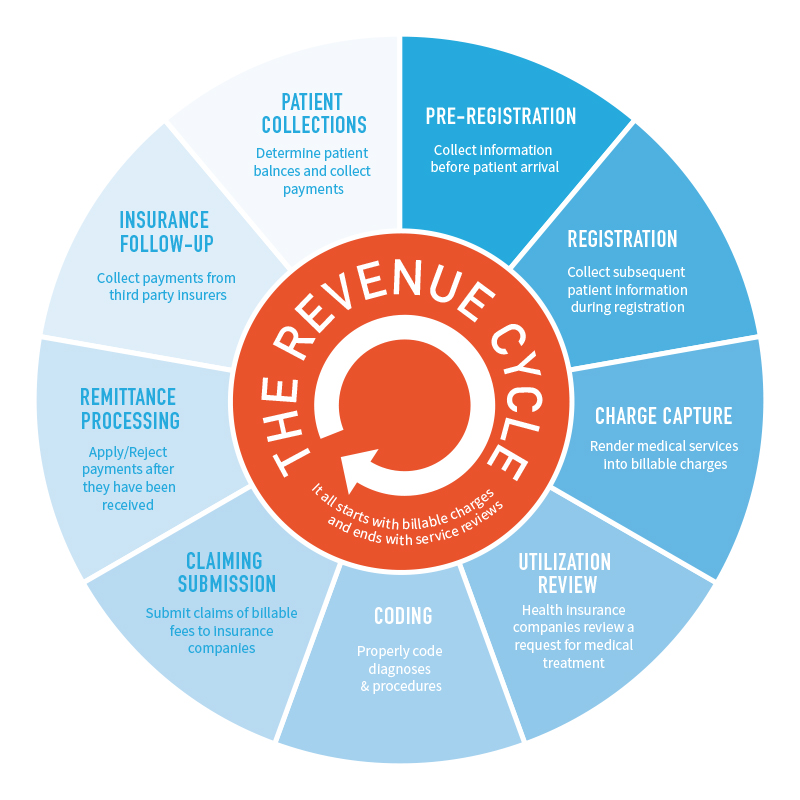
Pre-Registration & Registration
From the very beginning of patient interactions, your revenue cycle is disrupted by things beyond your control, like “No Show” appointments.
When a scheduled patient doesn’t arrive for their appointment, you lose time, money, and opportunity. Efficiency goes down while stress levels rise for everyone. Then, that patient’s medical care is now delayed.
What if you could reduce that number to less than 2% of your total appointments? Auto scheduling, auto patient contacts, and patient population dashboard monitoring are just the beginning of what robotic process automation can bring to your organization.
Digital workers can be set up as ChatBots and to do things like Text Messaging. This can streamline the scheduling and registration experience, improving your onboarding and intake processes almost immediately.
Content Services systems like OnBase integrate directly into leading Electronic Medical Records systems. With OnBase, you’ll have one central repository securely managing document storage from every step of the patient registration process, easily accessible from any authorized application in your system.
Charge Capture
You need to ensure your clinicians are accurately documenting and charging patients for every service they provide. For many years, your team has worked to catch omissions and errors downstream from treatment, hoping that by educating clinicians and digitizing records, you can reduce lost revenue. Even if you’re seeing good results, you’re still throwing more time and money at these problems than you need to.
Automating your charge capture will free your staff to focus on other tasks that make better use of their talent and experience. As OnBase pulls charts from the EHR, it automatically introduces them into the billing workflow. From scanning the document to entering the charges via Bot, OnBase eliminates data entry errors, reduces the need for human intervention in the process, and gives you far greater insights into your revenue integrity via robust data analysis.
Utilization Review
As more and more of your revenue cycle management is focused on your relationships with major health insurance providers, the better you can streamline that relationship, the better you can anticipate your true revenue projections.
One of the greatest changes you can make to improve your efficiency, speed, and accuracy is in Utilization Management. Because OnBase can house all of the documents necessary for pre-authorizations and utilization reviews, you can provide instant access to appropriate third parties via ShareBase. And, it’s all HIPAA compliant, secure, and trackable in real-time.
Coding
Optimizing your coding will yield immediately tangible results for your revenue stream. You’ll reduce denial rates, accelerate payments, and capture the correct revenue. Your staff will be happier and your patients better informed about their own care options and cost of care.
If you’re already using third-party Computer Assisted Coding (CAC) applications like Optum and 3M, then it’s as simple as integrating OnBase with your existing systems. OnBase will house the documents and drive workflows that route and assign charts automatically, ensuring speed and accuracy you’re unlikely to achieve with even the best back office staff.
No matter how well you automate your revenue lifecycle, remittance processing will always be a tedious, manual step… right? After all, you’ve got to ensure each E835 you receive matches the E837 sent out to that payer – a deceptively nuanced process of understanding billing and accounts receivables, and probably something only your highly trained staff is capable of doing, one piece of paper at a time.
You already know the answer – your remittance processing can be automated, too! With optical character recognition (OCR), you’ll be able to scan and store paper EOBs that can be retrieved from within your billing software. OnBase can also ingest your 835 files and present them as “documents” that can be managed within your Healthcare Information Management System like anything else.
The RPA digital worker can then strip off the authorization payment, send it to the bank for authorization, open the resulting payment drop box and determine payment and patient responsibility. Start to finish, your remittance processing just got easier, smarter, and faster.
Claiming Submission
If you’ve already modernized your coding processes, the next logical step is to extend that efficiency to Claims Submissions. You’re probably already closing out patient charts faster through automated deficiency management, but now your Claims team is the bottleneck. But it doesn’t have to be!
With OnBase acting as a “clearinghouse” for claims, a Robotic Process Automation digital worker can instantly and accurately verify claims eligibility and status via claims image searching.
Then, via the integrations with your third-party billing software that are already streamlining the rest of your revenue cycle, you can introduce RPA efficiencies straight from claims to billing without manual re-entry. Your team is relieved of the tedious re-entry and able to focus on patient satisfaction and billing efficiency, providing human intervention only where necessary.
Remittance Processing
No matter how well you automate your revenue lifecycle, remittance processing will always be a tedious, manual step… right? After all, you’ve got to ensure each E835 you receive matches the E837 sent out to that payer – a deceptively nuanced process of understanding billing and accounts receivables, and probably something only your highly trained staff is capable of doing, one piece of paper at a time.
You already know the answer – your remittance processing can be automated, too! With optical character recognition (OCR), you’ll be able to scan and store paper EOBs that can be retrieved from within your billing software. OnBase can also ingest your 835 files and present them as “documents” that can be managed within your Healthcare Information Management System like anything else.
The RPA digital worker can then strip off the authorization payment, send it to the bank for authorization, open the resulting payment drop box and determine payment and patient responsibility. Start to finish, your remittance processing just got easier, smarter, and faster.
Insurance Follow-Up
Claims and remittance processing aren’t the end of the billing cycle. There’s almost always additional resolution needed with your insurance partners, particularly for procedures that have been declined. Today, that may look like a very manual, paper-intensive process.
Tomorrow, it could look like an easy, digital workflow. Using RPA, a digital worker pulls the patient’s Continuity of Care document from OnBase and notifies a second Doctor that review is needed. That way, you can quickly, and effortlessly, verify if the procedure that took place is justified. Then, workflow can help manage the process for claims that have been denied, including managing the additional documentation and communication needed to resolve the specific case.
Patient Collections
Finally, your revenue cycle management ends with collecting the outstanding revenue from patients. And, you’ve probably already got a good system in place for that. Likely, it’s one of the first things you modernized to Software-as-a-Service (SaaS), and it runs great for what you need.
But, OnBase can come alongside your existing collections platform and offer several key benefits that streamline what may still be manual processes for your billing team. You can automate a system to read physical checks and then leverage an RPA digital worker to enter that data directly into your billing system.
When you sell an account to an agency, you can leverage OnBase’s document management to package all relevant billing files and submit them seamlessly via an RPA workflow, making the collections process a smooth running revenue engine.
Between automation technology like Capture, RPA and OnBase ECM, KeyMark has your revenue cycle management covered. Contact us today!
Contact us today to start the conversation!
No pressure. Let’s see if automation technology is a fit your your healthcare organization. We can talk through next steps, like budget parameters and timeline.